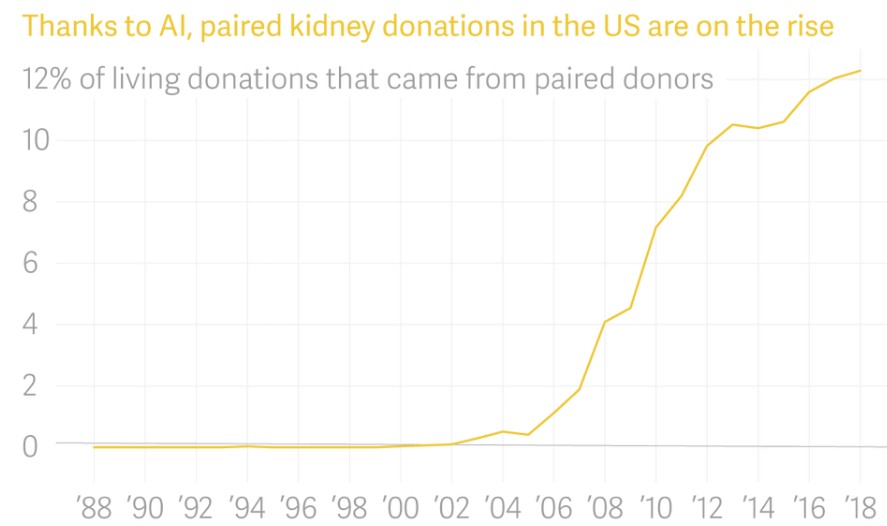
In the past, there were only three ways to get off the waiting list for a kidney transplant. The first is to find a healthy person from your friends and family, who perfectly matches the recipient's blood and tissue type, and has a spare kidney that he or she is willing to give up. The second is to wait for a stranger to die unexpectedly. This stranger is a suitable physical match who happened to have selected organ donation on their driver's license. The third is death. But then the doctors thought: With enough kidney patients and enough healthy voluntary donors, they can form a large enough donation pool to promote more matching than in the past one-to-one system. As long as the patient can find a donor—any donor, even if it’s a mismatched patient—they can get a matching kidney. At first, this required doctors to spend several hours carefully studying the details of blood type and tissue changes in the patient and potential donor list. Then, computer scientists and economists got involved. The algorithms they built perform these complex matches more elegantly than the human brain. Now, thanks to artificial intelligence, one person taking the courageous step and donating a kidney to a loved one—or a complete stranger—can open a chain that saves dozens of lives. Matched kidney donation is one of the great success stories of artificial intelligence. This does not eliminate work, nor does it erase the human touch in healthcare. It tackled a very complex problem, solved it faster than humans, made fewer mistakes, and saved more lives. Since the start of the first pair of kidney exchange surgery in 2000, nearly 6,000 people have received paired exchange kidney transplants identified by algorithms. Today, approximately one-eighth of transplant recipients who receive a kidney from a living donor are paired with that person through a pairing exchange. At the same time, paired kidney exchange is also a perfect example of the limitations of artificial intelligence. Computers can only do what humans can teach it, and we cannot teach what we don't understand. In the decades since the medical learned how to replace failing kidneys with donated kidneys, we are still trying to solve the problem of how to distribute the precious small amount of kidneys. This distribution method makes everyone feel fair and satisfied, and does not lead to undesirability. Unintended consequences. Artificial intelligence can identify potential donors and recipients that are biologically suitable for each other; in the future, it can even weigh the moral factors that determine who receives the transplant first. But first, we humans must agree on what these should be. The kidney acts as a filter for the body. For people with kidney failure, dialysis basically replicates the function of the organ from the outside, draining the patient's unfiltered blood for several hours, and then pumping it back into the body. The invention of dialysis in the mid-20th century turned a disease that was once a death sentence into a chronic but manageable disease. The first outpatient dialysis center, Seattle Artificial Kidney Center, opened in January 1962. Because each patient needs to be treated on the machine twice a week for 12 hours, the center can only accept 10 of the approximately 2,000 American patients with end-stage renal disease who were eligible for dialysis during the first two years. In order to take profits in its own hands, the center organized an independent committee of seven citizens. The first acceptance and policy committee — or later called the "God Committee" by the media — consisted of a lawyer, pastor, banker, housewife, state official, labor leader, and surgeon. The doctor made some decisions for them: patients over 45 years old are not eligible, and children are not eligible, because the doctor is worried that the operation may bring them mental trauma. In addition, the committee can select about a quarter of eligible applicants. According to an article in "Life" magazine in 1962, the members of the anonymous committee consider the age and gender of the applicant, and whether they are married or have children. They will consider the applicant's emotional stability. They will look at how much money applicants make and how much money they have saved; their education level, job, past behavior and future potential. They decided that since the research to develop the technology was conducted in Washington State-funded institutions, only Washington residents would be considered because the state's taxes were paid for the treatment. The article stated that committee members as "noble-minded and kind citizens" face an almost impossible task. They are also humans, and as humans, they are always affected by conscious and unconscious biases. They make decisions based on medical records written by doctors, and doctors have conscious and unconscious biases. The seven members of the committee are part of the upper-middle class in the Pacific Northwest of the United States, and their discussions (at least those published publicly) hint at favors for patients who seem to share their status and values. Race is never mentioned in Life magazine, but it’s hard to imagine that in a society that is still severely segregated (just to give one example, 98% of Washington State employees at the time were white), people of color are not considered by these representatives Among. Their discussion foreshadows a problem that will last a long time before the original kidney treatment machine is surpassed by more advanced technology. Even if a group of people agree to do the best thing possible, what is the best thing for most people? When the Council of God issued its painful decision, similar work was being done to treat patients with kidney disease elsewhere. In 1954, the doctor performed the first successful kidney transplant operation at Birghamand Women's Hospital in Boston. An organ was surgically removed from a 23-year-old man and transplanted to his twin brother. The recipient survived. For eight years. By the early 1960s, the development of blood and tissue typing made it easier for doctors to identify successful matches between donors and recipients, and improvements in immunosuppressant drugs have greatly reduced the rate of transplant rejection. Today, the kidney of a deceased donor will continue to work in the recipient's body for 8 to 12 years, while the average life span of a kidney from a living donor is 12 to 20 years. In 1972, US President Richard Nixon signed legislation to expand medical insurance coverage to include dialysis for all kidney failure patients. Dialysis did not cure them, but it allowed more people to survive longer while waiting and hoping for a kidney transplant. Since then, the number of people requiring kidney transplants in the United States has grown much faster than the number of available donors. According to the Organ Sharing United Network, as of this writing, 114,554 people in the United States are waiting for organ transplants. Of these, 94980-83%-are waiting for a kidney transplant. The Uniform Anatomical Donation Act of 1968 established a standard procedure in the United States through which people or their close relatives can authorize the donation of their organs after death. However, even if everyone in the United States is a registered organ donor (the current ratio is 54%), there are not enough kidneys to meet the demand. Less than 2% of people die in a way that makes them suitable organ donors. Organs can still be transplanted after a person's death, and oxygenated blood must be continuously pumped through them until they are removed from the body by surgery. Before the harvesting operation, the deceased donor is usually declared brain dead and connected to a ventilator. Fortunately, since most people are born with two functioning kidneys and only need one to survive, people who are alive can donate kidneys. Since living donors often live longer kidneys than deceased ones, finding a living donor is usually the ideal result for people in need of transplantation. Although all operations have the risk of complications or death, most kidney donors only need to stay in the hospital for two or three days after laparoscopic surgery, followed by another four to six weeks of recovery time. The remaining kidney will develop to compensate for the donated kidney, and the donor will usually continue to lead a normal life. Of course, applying for organs to your siblings is not a trivial matter. But finding someone who is willing to donate is usually the easiest part of the process, because many patients and their families will find it impossible to match organs. Florida businessman Neil Emmott was diagnosed with polycystic kidney disease in 2001, a genetic disease that can lead to kidney failure. His wife Lisa Emmott said the news was "unexpected and devastating." At the time of diagnosis, Neil was 38 years old and Lisa was 27 years old. The couple had been married for less than a year. By 2016, they had two young daughters, and Neil's condition deteriorated to the point where doctors at Johns Hopkins University advised him to consider transplant options. Lisa volunteered to donate immediately. She is healthy and has the same blood type as him, so she considers herself a viable candidate. But organ donation requires more than blood and tissue matching. Donors need to be thoroughly screened. Psychological or socio-economic issues may complicate their donations. Lisa learned that a benign abnormality in the shape of her renal arteries—the veins that carry blood in and out of the kidneys—disqualified her. Neil's brother played as a substitute, but was also excluded due to some minor medical issues. The family felt very sad. "Needing organs is a terrible thing," Emmott said. At this time, the family decided to seek the market. The idea of ​​a "market" for human organs is creepy. They are not commodities: American law explicitly prohibits the sale of human organs. But from an economic point of view, the market is where anyone who wants something finds someone who can give them something. This market that does not rely solely on prices to allocate resources is called a matching market. Dating pools are a type of matching market (assuming no money is used to exchange friendships); the same is true for people who want kidneys and people who are willing to donate kidneys. The market works best when the market is "thick" or there are many participants. In the first few decades of kidney transplantation, sick people and their potential donors were confined to their own very weak market. A failed match often turns out to be a death sentence for a seriously ill patient. But what if the market can become thicker? This idea was first proposed in a paper by Felix Rapaport, a German-American surgeon in 1986. He proposed a theory that a kidney can be transplanted across two voluntary donor and recipient pairs: Patient A receives kidney from donor B as Exchange, donor A gives patient B a kidney. In 1991, doctors in Seoul, South Korea, under the guidance of kidney specialist KiilPark, performed the first pair of kidney transplants between two donor-patient pairs. Four years later, the world's first matched kidney donation project was launched in Seoul Yonsei University School of Medicine. Potential donors and recipients are entered into a database and then manually matched by doctors through hours of painstaking analysis. In 1999, Switzerland became the next country to establish a paired kidney exchange, matching two married couples, each of which had a spouse with end-stage renal disease and a spouse who was willing to donate kidneys. One night in 2000, after being tired of delivering heartbreaking news to patients and their loved ones, an American nephrologist named Michael Rees dragged a few boxes of documents home and spent several hours carefully examining the blood, Antibody and tissue data, and compare patient lists. This work is mentally tiring. In the end, he realized that he had no viable match-but if the donation pool was larger, he could make a match. Working with his father Alan Rees (Alan is a computer scientist), Michael Rees created a simple computer program to pair donors with recipients, introducing artificial intelligence into the matching process. Around the same time, Alvin Roth, a professor of economics at Harvard University, was also tinkering with the solution for kidney matching. Roth focuses on market design, focusing on how to adjust the market to repair the imbalance between supply and demand. He has previously designed algorithms to match new doctor and resident programs, as well as elementary and high school students in New York City. Now he turned his attention to the kidneys. Roth and his colleagues UtkuUnver and TayfunSonmez designed an algorithm to review and analyze data from potential donors and recipients. It defines the "cycle" and "chain" of donor-recipient pairings, in which one person chooses to selflessly donate his kidney to anyone who needs a kidney, thus among the potential donors and recipients registered in the hospital or kidney exchange program A series of donations were initiated. For example: Patient B gets a kidney from altruistic donor A, and then donor B gratefully donates the kidney to patient C. If patient C has a person who is willing to donate, then the chain can be extended without real restrictions. Unlike the cycle, the chain can move forward indefinitely without having to go back, ending the cycle by finding the kidney for the partner recipient of the original donor. Roth, Unver, and Sonmez think they are doing something big. In 2003, they published a paper outlining their work on the Internet and sent it to nephrologists across the United States. Based on feedback from Harvard surgeon Frank Delmonico, the team adjusted their algorithm and published a new paper whose concept helped establish the New England Kidney Exchange Project. The exchange program matched donors and recipients from 14 kidney transplant centers in the region. At first, the surgeon insisted on performing all the operations at the same time in a given loop or chain, so that no donor would back down at the last minute. This limits the number of patients in the loop or chain because the hospital can only free up so many beds and so many surgeons at a time. Economists and several other doctors believe that this is an unnecessary restriction. There are no biological barriers: unlike the heart or lung, the heart or lung must be transplanted within 4 to 6 hours after leaving the donor's body, and the kidney can be safely stored for 24 to 36 hours before a new host is found. As for the possibility of weak links in the donor chain, economists believe that in a chain that starts with donors who are willing to give kidneys to anyone, if the donor shrinks, no recipient will be helpless, because doctors can Alternatives can be found in the registered donor library. Rees, a nephrologist who built the first matching algorithm, proved that it can be done. After a 28-year-old donor provided a kidney to a stranger in need, Rees organized a series of kidney donations that saved the lives of 10 patients in five states in eight months. Today, many hospitals in the United States have their own matching kidney donation programs. In addition, there are three larger inter-hospital kidney exchange programs in the United States: the Joint Organ Sharing Network, the National Kidney Registry, and the Matched Kidney Donation Alliance. There are national exchange programs in the United Kingdom, Canada and the Netherlands, and matching donations occur in hospitals from India to South Africa. The researchers also inferred that lung and partial liver transplantation may also undergo similar exchanges, although there is no such exchange system yet. In 2012, Roth won the Nobel Prize for his work in market design. He took Rees to the ceremony. By then, 2,000 people in the United States had received the transplant, which was the result of the system they helped create. Thousands of people have been helped since then. NeilEmmott eventually became one of the eight people in the 2017 Kidney Chain, which began when two family and friends came to donate to him. On August 13, 2018, a woman in Alabama became the 100th person to receive a kidney transplant in the nationwide donation chain since 2013. Today, when doctors are looking for matching kidney donors and recipients, algorithms built by artificial intelligence researchers search the database of registered kidney patients and their co-donors, and based on the weights established by the Organ Procurement and Transplant Network Committee and the Organ Sharing Joint Network A list of criteria to identify matches. These algorithms simultaneously evaluate all possible transplants in the patient-donor bank. Matching is mainly based on biocompatibility, and the patients who are the most difficult to match are given priority. This technology measures the time the recipient has been on the waiting list, his or her age (child priority), and whether the person in need of a kidney has been a living organ donor in the past. These algorithms have helped thousands of life-saving operations. In the future, artificial intelligence can not only use human-decided criteria for matching, but also actively participate in this judgment process-understanding human decisions and value systems, so that it can make its own judgments and decide which kidneys should go and where (this decision Will be reviewed by a human doctor). At this point, the limiting factor is not so much technology as the people who use it. The first problem is human anxiety about the role of artificial intelligence in organ allocation. Hospitals and organ exchange organizations are not even willing to use the term "artificial intelligence" in the matching process. Part of the reason is a trend that researchers call the "artificial intelligence effect." As Nick Bostrom, director of the Institute for the Future of Humanity at the University of Oxford, said, “Once something becomes useful and common enough, it will no longer be labeled as'artificial intelligence'.†In view of the lack of public education on the actual meaning of "artificial intelligence", hospitals and exchanges are cautious about patients' misunderstanding of the role of algorithms in identifying potential matches, perhaps because they are afraid of juggling robots coldly issuing life and death instructions. Currently, the machine cannot decide which kidneys go where. Humans can do this. Today's algorithms are more reliable than humans, and they perform mathematical operations on a larger scale and perform judgments that humans have already made, but they do not understand why calculations are performed in the first place. "AIs don't have a comprehensive understanding of the world like we do. They don't understand what the data they are processing is about," said Vincent Conitzer, professor of computer science, ethics and philosophy at Duke University. "They don't have the concept that this person is suffering. They don't really understand what a person is. Humans must step in at some point." Researchers are now teaching machines to understand these moral dilemmas from a human perspective. This year, Conitzer and Duke University colleagues Jana Schaich Borg, Walter Sinnott-Armstrong, Rachel Freedman, and John Dickerson of the University of Maryland published a paper in which they presented hundreds of hypothetical patient profiles to the research subjects and asked which of each pair was One should get a usable kidney. These hypothetical patient files did not list the blood and tissue data processed by the algorithm, but listed things such as how often the patients drank alcohol and whether they had had cancer in the past. The researchers then feed back the subject's choices to an algorithm and learn how to select the "correct" kidney recipient based on these patterns. Just like human subjects, artificial intelligence prefers younger and healthier patients-this is an example of a machine making decisions based on its understanding of human values. Although it is possible to teach machines to match according to our value system, we do not always understand what our values ​​are, or it is difficult to agree on them as a whole. People don’t always know what they want to optimize, and even when they think they have done so, they often don’t understand how to do it in a way that does not lead to unintended consequences. For example, MIT’s ethical machine allows visitors to the laboratory’s website to play the game they must choose. Under one hypothetical scenario after another, the driverless car should choose which one to kill when faced with two terrible choices. Group of car passengers or pedestrians. After going through a series of nauseating scenes-yes, I would rather car run over a pregnant woman than five homeless adults; no, if it means killing five adult passengers, I Don't turn suddenly to avoid two kids-this game reveals the patterns it determines in your choices and how your reactions compare to the reactions of other players. This information can reveal unexpected consequences and unpleasant unrecognized biases. For example, you may learn that your decision disproportionately caused more male deaths than females, or that you tend to value observing traffic rules more than the average player in the game. When it comes to kidney problems, it is to adopt the superficially fair principle, that is, the kidney should be given to those who may have the longest life expectancy after receiving the kidney. Before computers can calculate the life expectancy of potential recipients, scientists must provide algorithms with life expectancy data for various populations. But this caused some problems. Men tend to die earlier than women. Black Americans died earlier than Americans of any other race. In 2015, a 65-year-old white American woman may live another 20.5 years, 4 years longer than a black woman of the same age. Although it started with good intentions, it eventually led to systematic racial and gender discrimination. "In economics, we talk about impossibility theorems. There are things you might want but can't get," Roth said. "When you allocate scarce resources, you cannot give the kidney to one person without giving it to another. Computers will not reduce the burden on humans in every way." Artificial intelligence has not caused these moral dilemmas. The Human Committee is constantly troubled by the fairest way to allocate kidneys; human drivers still have to make terrible emergency decisions behind the wheel. Machines can simulate the results of human judgments within hours or even minutes. These results may have taken years to discover. In the long run, this may help: if a computer model can prove that a particular kidney allocation policy will have a disproportionately adverse effect on certain groups, then doctors can cancel the plan before anyone is actually harmed. But not everyone is happy to allow machines to participate in life and death decisions. The moral machine teaches players something that the Seattle Council of Gods learned a long time ago: you have to choose which life to save, knowing that this decision will lead to the death or suffering of others, it feels terrible. This part cannot be helped by artificial intelligence. People can find the ideal way to assemble chairs, and then teach this process to a machine that can perfectly assemble thousands of chairs. But there is no perfect way to decide who lives and who dies. Hybrid Split Phase Solar Inverter Shenzhen Jiesai Electric Co.,Ltd , https://www.gootuenergy.com